BackTable / VI / Tool
NIH Stroke Scale
The NIH Stroke Scale (NIHSS) is a standardized neurologic exam used to evaluate the severity of stroke-related deficits. Developed by the National Institute of Neurological Disorders and Stroke (NINDS), the tool assesses multiple domains of brain function including consciousness, vision, movement, sensation, language, and neglect. It is widely used in both prehospital and in-hospital settings to guide acute stroke care and treatment decisions.
The NIHSS stroke scale provides a reproducible method to quantify stroke severity and monitor neurological changes over time. Clinicians use the NIHSS score not only at presentation but also during hospitalization and recovery. It supports early decision-making, especially when evaluating patients for thrombolysis or endovascular intervention. While the scale is most accurate in anterior circulation strokes, it remains a core component of stroke assessment protocols across practice settings.
1a) Level of Consciousness
Assess level of consciousness even if the patient cannot respond verbally due to intubation, trauma, or language barriers. Choose the most appropriate score based on observed responses. Assign a score of 3 only if the patient shows no purposeful movement and responds to noxious stimuli with only reflexive or postural reactions.
1b) Level of Consciousness (Month & Age)
Ask the patient to state the current month and their age. Answers must be exact; no partial credit is given. Score 2 for aphasic or uncomprehending patients. Score 1 if speech is impaired by non-aphasic causes. Only the first response counts. Do not assist with verbal or non-verbal cues during assessment.
1c) Level of Consciousness (Commands)
Ask the patient to open and close their eyes, then grip and release the nonparetic hand. Substitute if needed. Give credit for clear effort, even if incomplete. If no response, demonstrate the task. Score based on response to initial attempt. Adjust commands for physical limitations such as amputation or trauma.
2) Gaze Deviation
Only horizontal eye movements are tested, using voluntary or reflexive (oculocephalic) responses. Caloric testing is not used. Score 1 if conjugate deviation is overcome or if an isolated CN III, IV, or VI palsy is present. Aphasic patients can be assessed. For trauma, blindness, or visual field deficits, use reflexive movements. Move side to side after eye contact to help detect subtle gaze palsy.
3) Visual Fields
Test visual fields in both upper and lower quadrants using finger counting or visual threat. Encourage the patient if needed. If they look toward the moving fingers appropriately, consider it normal. In cases of unilateral blindness or enucleation, test the remaining eye only. Score 1 if a clear asymmetry or quadrantanopia is found. Score 3 if the patient is completely blind from any cause. Perform double simultaneous stimulation to assess for extinction. If extinction is present, score 1 and use this finding when scoring #11.
4) Facial Palsy
Use voice or pantomime to encourage the patient to show teeth, raise eyebrows, and close eyes. In non-responsive patients, assess symmetry with noxious stimuli. If facial assessment is limited by trauma, tubes, or bandages, remove obstructions if possible to allow evaluation. Score based on movement and symmetry of facial response.
5a) Left Arm Motor Function
Position the left arm with the palm facing down, 90 degrees if sitting or 45 degrees if lying down. Test the left arm after the right. The patient must hold the arm up for 10 seconds. Score drift if it falls before then. Encourage aphasic patients with voice or gestures only. If testing is not possible due to amputation or joint fusion, mark as untestable.
5b) Right Arm Motor Function
Position the right arm with the palm facing down, 90 degrees if sitting or 45 degrees if lying down. Test the right arm first. The patient must hold the arm up for 10 seconds. Score drift if it falls before then. Encourage aphasic patients with voice or gestures only. If testing is not possible due to amputation or joint fusion, mark as untestable.
6a) Left Leg Motor Function
Position the left leg at 30 degrees while the patient lies supine. Score drift if the leg falls before 5 seconds. Encourage aphasic patients with voice or pantomime only. If testing is not possible due to amputation or hip joint fusion, mark as untestable.
6b) Right Leg Motor Function
Position the right leg at 30 degrees while the patient lies supine. Score drift if the leg falls before 5 seconds. Encourage aphasic patients with voice or pantomime only. If testing is not possible due to amputation or hip joint fusion, mark as untestable.
7) Limb Ataxia
This item checks for unilateral cerebellar lesions. Test with eyes open, ensuring the visual field is intact if deficits are present. Perform finger-nose-finger and heel-shin tests on both sides. Score ataxia only if it is out of proportion to weakness. Do not score if the patient is paralyzed or cannot understand. If amputation, joint fusion, or blindness prevents testing, mark as untestable and explain the reason.
8) Sensory
Assess sensation using pinprick or response to noxious stimuli, including withdrawal or grimace in aphasic or obtunded patients. Test multiple areas (arms, legs, trunk, face) to confirm hemisensory loss from stroke. Score 2 only for clear, severe or total sensory loss. Bilateral loss from brainstem stroke, quadriplegia, or coma (#1a=3) also scores 2. Aphasic or stuporous patients typically score 0 or 1.
9) Best Language
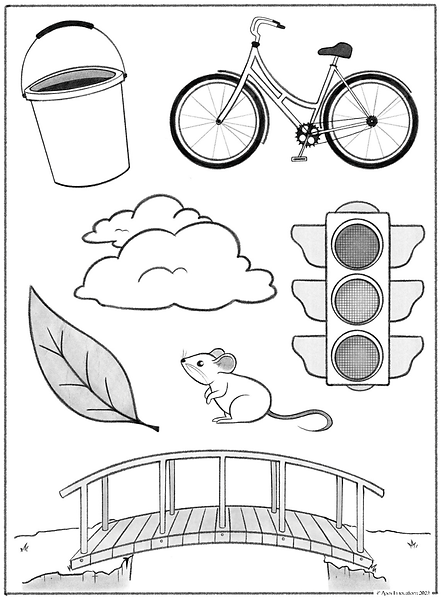
Comprehension is assessed using both earlier exam interactions and specific tasks in this section. Ask the patient to describe what is happening in Best Language Image 1 (see below), name objects in Best Language Image 2 (see below), and read the sentences in Best Language Sentences (see below). Evaluate comprehension based on these tasks and the patient’s ability to follow previous commands.
If visual loss interferes with testing, ask the patient to identify objects placed in the hand, repeat spoken words, or produce speech. Intubated patients should be asked to write. Patients in a coma (#1a=3) automatically receive a score of 3. For patients with stupor or limited cooperation, choose the most appropriate score based on available responses. A score of 3 should only be used if the patient is mute and does not follow even simple one-step commands.
10) Dysarthria
If speech appears normal, confirm by having the patient read or repeat words from the list Dysarthria Words (see below). For severe aphasia, assess clarity of spontaneous speech. Only mark as untestable if the patient is intubated or has a physical barrier to speaking. Do not explain the purpose of the test.
11) Extinction and Inattention (Neglect)
Evaluate extinction and inattention using information from prior testing. If the patient cannot undergo visual double simultaneous stimulation due to severe visual loss but responds normally to touch, score as normal. Aphasic patients who attend to both sides are also scored as normal. Evidence of visual neglect or anosognosia indicates abnormality. This item is scored only if abnormal and is never marked untestable.
Value 1
Value 2
Best Language Image 1

Best Language Image 2
Best Language Sentences
• You know how.
• Down to earth.
• I got home from work.
• Near the table in the dining room.
• They heard him speak on the radio last night.
Dysarthria Words
• MAMA
• TIP-TOP
• FIFTY-FIFTY
• THANKS
• HUCKLEBERRY
• BASEBALL PLAYER
• CATERPILLAR
Clinical Use of the NIH Stroke Scale
The NIHSS is typically administered upon initial evaluation of suspected stroke. EMS providers, emergency physicians, neurologists, and stroke teams use the scale to stratify severity and inform triage decisions. NIHSS scoring ranges from 0 to 42:
• 0: No stroke symptoms
• 1–4: Minor stroke
• 5–15: Moderate stroke
• 16–20: Moderate to severe stroke
• 21–42: Severe stroke
A score of 0 indicates no observable neurologic impairment, while scores above 20 often correspond with large vessel occlusion or extensive infarction. NIHSS scores are routinely used to assess eligibility for IV thrombolysis, typically within a 0–25 range. While no absolute cutoff exists, lower scores may prompt reevaluation of symptom severity, and higher scores may increase concern for hemorrhagic risk. For mechanical thrombectomy, moderate to severe scores (generally NIHSS ≥6) often trigger vascular imaging to assess for large vessel occlusion. Patients with favorable imaging profiles, such as small infarct core and salvageable penumbra, are considered strong candidates for endovascular therapy.
Additionally, the NIHSS helps predict outcomes. Lower scores on admission generally correlate with better functional recovery. Repeated NIHSS assessments during hospitalization can identify early neurologic deterioration or improvement, influencing medical management and prognosis discussions.
Interpretation & Scoring Domains
The NIHSS includes 11 components that evaluate key neurologic functions:
1. Level of consciousness (LOC)
2. Gaze Deviation
3. Visual Fields
4. Facial Palsy
5. Arm Motor Function
6. Leg Motor Function
7. Limb ataxia
8. Sensory
9. Best Language
10 Dysarthria
11. Extinction and Iinattention (neglect)
Each item is scored individually and contributes to the total score. Scoring varies by domain, with some ranging from 0 to 2 and others up to 4. Higher scores reflect more significant impairment. Consistent training is required to ensure accurate scoring, especially when clinical findings are subtle or subjective.
While comprehensive, the NIHSS may underrepresent posterior circulation strokes, which often involve symptoms like dizziness, nausea, or ataxia that are either minimally weighted or not included. For this reason, imaging and broader clinical context should always accompany NIHSS interpretation.
Limitations & Clinical Considerations
Despite its wide use, the NIH Stroke Scale is not without limitations. It places greater emphasis on language and motor deficits typically seen in left hemispheric and anterior circulation strokes. Posterior strokes, which may present with symptoms like diplopia, dysphagia, or truncal ataxia, are not fully captured by the NIHSS, potentially leading to underestimation of severity.
Interrater variability is another concern, particularly with components like neglect or dysarthria, which rely on subjective interpretation. Proper training and regular calibration among team members help improve reliability. Clinicians should also consider that the scale was not designed to guide long-term prognosis and may not reflect cognitive or functional impairments seen during recovery.
For comprehensive guidance on NIHSS use and scoring criteria, clinicians are encouraged to refer to official resources from the National Institute of Neurological Disorders and Stroke.
Learn more on the BackTable VI Podcast
BackTable is a knowledge resource for physicians by physicians. Get practical advice on the NIH Stroke Scale and how to build your practice by listening to the BackTable Podcast.
References
[1] Durand, F., & Valla, D. (2005). Assessment of the prognosis of cirrhosis: Child–Pugh versus MELD. Journal of Hepatology, 42(1). doi:10.1016/j.jhep.2004.11.015
[2] Tsoris, A. (2020, May 17). Use Of The Child Pugh Score In Liver Disease. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK542308/
[3] Molla, N., AlMenieir, N., Simoneau, E., Aljiffry, M., Valenti, D., Metrakos, P., Boucher, L. M., & Hassanain, M. (2014). The role of interventional radiology in the management of hepatocellular carcinoma. Current Oncology, 21(3), e480–e492. https://doi.org/10.3747/co.21.1829
Disclaimer: The Materials available on BackTable.com are for informational and educational purposes only and are not a substitute for the professional judgment of a healthcare professional in diagnosing and treating patients. The opinions expressed by participants of the BackTable Podcast belong solely to the participants, and do not necessarily reflect the views of BackTable.


